REBEL-EM is a fantastic source of blogs and podcasts, helping you to stay in touch with the latest mutterings in the hallways of EM......Check it out for the proper post with all the images!
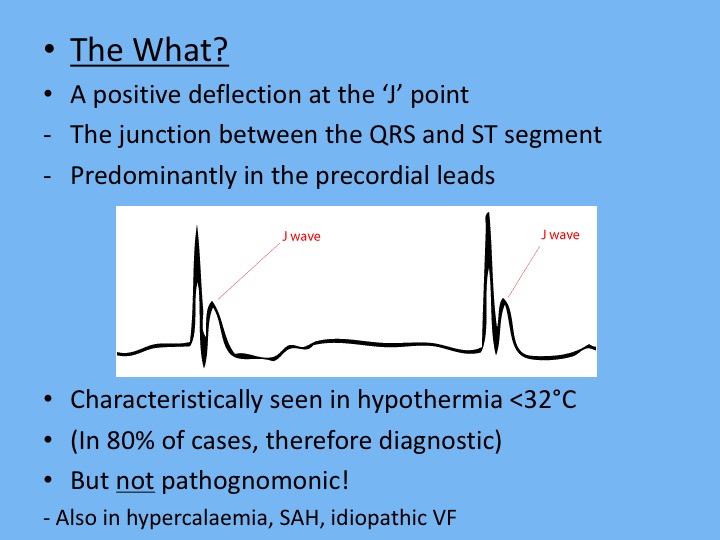
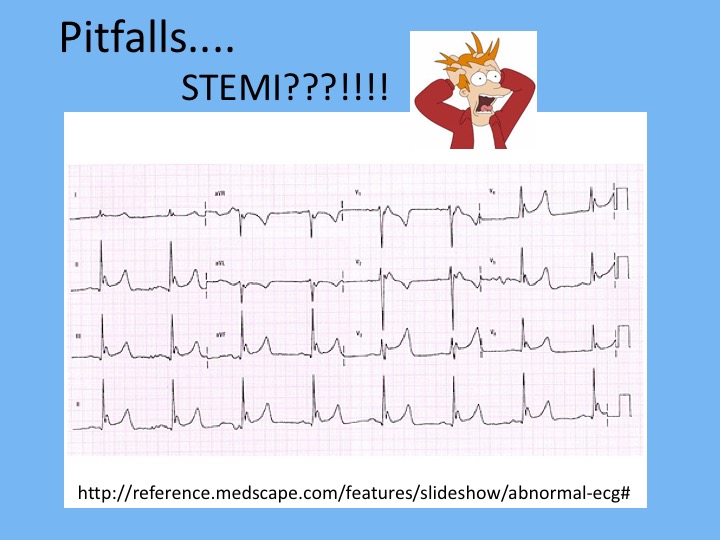
Background: The electrocardiogram (ECG) is one of the most useful diagnostic studies for identification of acute coronary syndrome (ACS) and acute myocardial infarction (AMI). The classic teaching is ST-segment elevation myocardial infarction (STEMI) is defined as symptoms consistent with acute coronary syndrome (ACS) + new ST-segment elevation at the J point in at least 2 anatomically contiguous leads of at least 2mm (0.2mV) in men or at least 1.5mm in women in leads V2 – V3 and/or at least 1mm (0.1mV) in other contiguous leads or the limb leads, in the absence of a left bundle branch block, left ventricular hypertrophy, or other non-acute MI ST-segment elevation presentations. Unfortunately, the ECG may be non-diagnostic in nearly half of all patients who initially present with AMI. There are also STEMI equivalent patterns that are caused by occlusion of the coronary arteries that place a significant portion of the left ventricle at jeopardy and result in poor outcomes. This review article focused on 5 under recognized high-risk ECG patterns in the ACS patient that result in poor outcomes including malignant dysrhythmias, higher rates of cardiogenic shock, and death.
First Diagonal Branch of the Left Anterior Descending Artery Occlusion
- The 1st diagonal branch (D1) of the LAD supplies blood to the anterolateral wall of the left ventricle
- Look for:
- STE in aVL and V2
- Upright T-waves in aVL and V2
- ST-Depression and inverted T waves in Inferior Leads (III and aVF)
- STE in aVL and V2 + lack of STE in other precordial leads = 89% PPV for MI of the anterior wall caused by a D1 lesion
De Winter’s T Waves
- Concerning for proximal LAD occlusion (Present in 2% of patients)
- Look for:
- Upsloping ST-Depression at J Point in leads V1 – V4 without STE
- Tall, Symmetric T-Wave in leads V1 – V4
- STE in lead aVR +/- aVL
Left Main Coronary Artery Occlusion
- Look for:
- STE in lead aVR AND/OR
- Widespread ST-Depression
- In one study STD in leads I, II, and V4 – V6 + STE in aVR present in 90% of patients with greater than 70% stenosis of the LMCA
Wellens’ Syndrome
- Concerning for proximal critical high grad LAD occlusion
- Consider Wellens’ if:
- Active (or recent) angina chest pain
- Minimal or no cardiac biomarker elevation
- Absence of pathologic precordial Q waves
- Minimal or lack of STE (<1mm)
- No loss of precordial R-wave progression
- Characteristic T-wave abnormalities
- Two Types of Wellens’ Syndrome:
- Type A (25% of cases) consists of biphasic t waves
- Type B (75% of cases) consists of deep symmetric t waves
- Provocative Stress Testing could prove to have disastrous consequences resulting in AMI and fatal dysrhythmias
- AMI can occur within a mean of 6 – 8.5d after admission, but a mean of 21.4d after symptoms
- T-wave changes may be transient or resolve with medical management
- Look for:
- Deeply inverted T-waves in leads V1 – V4 OR
- Biphasic T-waves in leads V1 – V4
Posterior Wall AMI
- Concerning for occlusion of either distal left circumflex artery or PDA of right coronary artery
- If you see STD in leads V1 – V3, the next thing to do is get a posterior ECG with leads V7 – V9 to help differentiate posterior AMI vs Anterior Ischemia
- Look for:
- Horizontal (flat) ST-Depression in leads V1 – V3
- Prominent R-wave in leads V1 – V2
- Upright T-wave in leads V1 – V3
Clinical Bottom Line: It is important to recognize the above 5 patterns as these are high risk ACS patients because a significant portion of the left ventricle is at jeopardy. Only 4 of the above diagnoses require activation of the cath lab immediately and the 5th requires consultation of interventional cardiology.
Cath Lab Activation:
- 1st Diagonal Branch of the Left Anterior Descending Artery Occlusion
- de Winter’s T Waves
- Left Main Coronary Artery Occlusion
- Posterior STEMI
Interventional Cardiology Consultation: